Model Demonstrates Cause of Heart Arrhythmia
An abnormal heart rhythm called atrial fibrillation (AF) can lead to a stroke, but physicians don’t understand exactly what causes it. A new mathematical model of the collective activity of heart muscle cells may improve understanding of this condition by representing the organization of cells in heart tissue more accurately than previous models. The new model agrees with earlier suggestions that the amount of communication between individual muscle fibers is a critical factor leading to AF, but it goes further by showing a direct cause-and-effect relationship. The work could inform surgical treatments in the future by suggesting exactly where problems lie in a given patient’s heart.
A healthy heart beats regularly as waves of electrical activity pass through the cardiac muscle, propagating from one muscle cell to another. If the coordination between cells breaks down, the electrical impulses in the tissue can become less regular, and the heart flutters more randomly. This state is atrial fibrillation, and it can lead to many serious symptoms, including stroke.
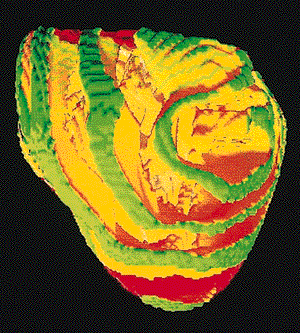
Previous work has suggested that AF is associated with a switch from ordinary electrical waves, propagating across the heart like linear wavefronts in water, to rotating and spiral-shaped wavefronts that curl out from a central point [1–3]. Rotating waves can be triggered in regions where the interactions between neighboring cells are abnormal—for example, in heart tissue with fibrosis, a condition where excess collagen reduces connections between adjacent muscle fibers. But exactly why such locations produce rotating waves hasn’t been clear.
The formation of wavefronts in heart muscle has often been studied using so-called cellular automata models, which treat the tissue as a grid of cells. Each cell is assigned a state of electrical activity—“excited” or quiescent—based on a rule that relates its state to those of its neighbors [2]. As the simulation runs, the cell states change over time and can develop spontaneous modes of organized activity involving many cells. Kim Christensen and co-workers at Imperial College in London have now devised a cellular automata model that more accurately captures the tissue structure of the heart.
Heart tissue is made up of strands of cylindrical muscle cells, with cells communicating mainly end-to-end and with much less side-to-side interaction. The model of Christensen and colleagues reflects this structure, arranging the cells into two-dimensional sheets of parallel strands. The amount of lateral coupling between neighboring strands is represented by a parameter ν, which turns out to be the critical factor for rotating waves to develop.
If ν is relatively large, then the model tissue develops healthy, linear waves. But if ν falls below some threshold value ( 20% in one case they studied), there is a sudden switch to a new state in which rotating waves form. Then the traveling waves of activity move mainly along the fibers, but with occasional jumps down to the next fiber and then back again in a loop. Sometimes this “re-entrant” AF state might last for only a short time before regular pulses resume, just as AF might be transient in real hearts. But sometimes it persists indefinitely in the model. Previous models required some kind of obstruction representing damaged tissue to produce these waves; the new model does it spontaneously, based solely on the value of ν.
This acute dependence on the lateral communication of fibers is consistent with what is found medically, as with fibrosis. So physicians might in principle want to measure ν to predict a patient’s AF risk. However, today’s MRIs aren’t up to that job, says graduate student team member Kishan Manani, although improved imaging technologies may allow such assessments in the future.
Some recent surgical treatments for AF involve using microwave radiation to ablate the areas of heart tissue in which the rotating waves are initiated. These can be regions where fibrosis has developed. Christensen and colleagues find that, if a rotating-wave-initiating, low- ν area of their model tissue is removed, leaving inert tissue, the AF state can be restored to a linear wavefront.
“This interesting study provides a conceptual framework that explains many observed features of human atrial fibrillation,” says cardiologist Sanjiv Narayan of Stanford University in California, who has experimented with the ablation approach. He adds that the ability of the model to predict the results of particular perturbations to heart structure, such as tissue ablation, remains to be demonstrated.
This research is published in Physical Review Letters.
–Philip Ball
Philip Ball is a freelance science writer in London. His latest book is How Life Works (Picador, 2024).
References
- R. A. Gray and J. Jalife, “Spiral Waves and the Heart,” Int. J. Bifurc. Chaos 6, 415 (1996)
- G. Bub, A. Shrier, and L. Glass, “Spiral Wave Generation in Heterogeneous Excitable Media,” Phys. Rev. Lett. 88, 058101 (2002)
- S. M. Narayan, D. E. Krummen, K. Shivkumar, P. Clopton, W. Rappel, and J. M. Miller, “Treatment of Atrial Fibrillation by the Ablation of Localized Sources,” J. Am. Coll. Cardiol. 60, 628 (2012)
More Information
Focus story on ways to interrupt rotating waves: Physics for “ER”