Can MRI Help Elucidate Iron-Based Neurotoxicity?
Iron plays a major role in life. Most obviously, it keeps us alive, helping to ferry oxygen around our bloodstreams. It is also essential in cellular energy production, in the immune-system response, and in brain function—where it helps catalyze the synthesis of dopamine and other neurotransmitters. Iron can, however, be a double-edged sword. An iron excess has been implicated in many ailments, including neurodegenerative conditions such as Alzheimer’s, multiple sclerosis, and Parkinson’s disease—where dopaminergic neurons (neurons that use iron to synthesize dopamine) degenerate. It is thought that the toxicity of iron depends on how it is stored: iron firmly bound within proteins such as ferritin may be less toxic than iron more loosely bound to low-affinity sites, where it is more able to participate in reactions that generate cell-damaging hydroxyl radicals [1]. But how can we tell, without removing the iron from its physiological environment, which binding state it is in? Now Malte Brammerloh of the Max Planck Institute for Human Cognitive and Brain Sciences in Germany and colleagues have demonstrated a new method for characterizing the form of iron binding at the single-cell, or single-neuron, level [2]. The results may improve our understanding of iron neurotoxicity and hold promise for facilitating the early detection of diseases such as Parkinson’s.
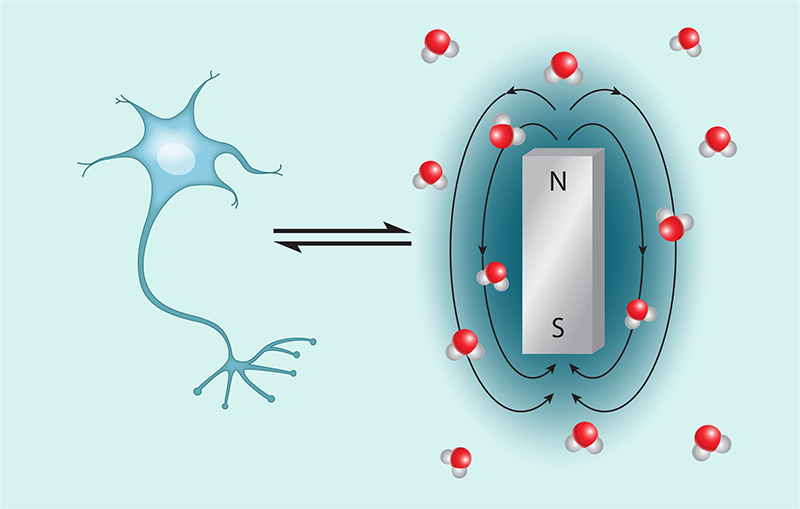
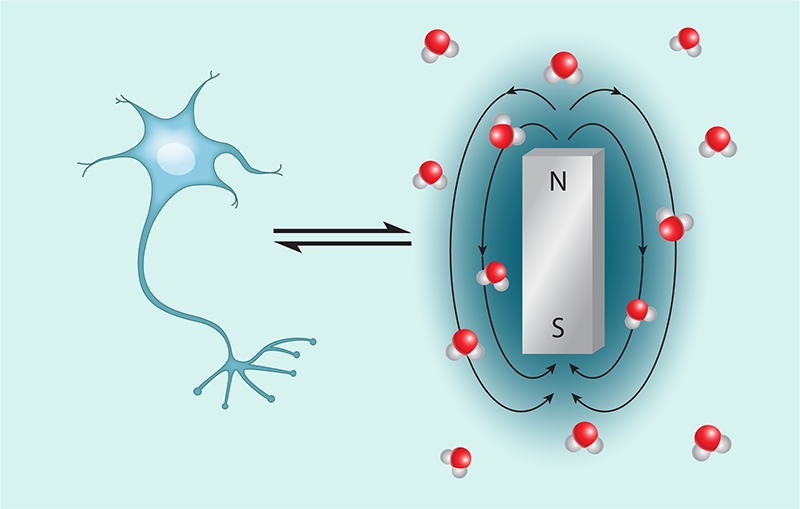
Magnetic resonance imaging (MRI) is a leading medical imaging tool, providing three-dimensional views of volumes deep inside our bodies. Being most sensitive to the spins of protons in hydrogen atoms, MRI primarily depicts the water distribution inside us. But it can tell us more than just where the water is or how much of it there is. With appropriate sequences of radio-frequency magnetic pulses, MRI can discern if that water is stationary or moving and determine its nuclear magnetic resonance (NMR) relaxation times. These two times, called T1 and T2, quantify how the magnetization induced in the sample by the radio-frequency pulses decays in directions that are, respectively, longitudinal and transverse to the MRI-field direction. The relaxation times depend on the surrounding tissue environment and, in particular, on spatiotemporal variations in the magnetic fields around the measured molecules. Thus, although MRI predominantly sees water, the presence of magnetizable metals such as iron, as well as the strength of the fields they generate, can be inferred through the changes in the water’s NMR relaxation times.
This ability of MRI to noninvasively detect the magnetic field of iron inside the body has enabled many brain-iron studies over several decades [3–5] but does not imply the ability to determine the binding form, hence the toxicity, of that iron. Fortunately, such information might be accessed by measuring magnetic susceptibility, which quantifies how easily a material becomes magnetized when exposed to a magnetic field. It is believed that tightly bound iron, such as that bound to ferritin, adopts a largely antiferromagnetic crystalline structure, yielding a lower magnetic susceptibility than that expected for iron more loosely bound to mononuclear low-affinity sites. This behavior suggests that stores of iron with different toxicities might be distinguished by their different magnetic susceptibilities. Naively, one might expect that this feat could be achieved with existing MRI techniques, such as quantitative susceptibility mapping [6, 7], that convert measured maps of magnetic fields into maps of magnetic susceptibilities. However, knowing the overall susceptibility of material in an imaged voxel (the three-dimensional equivalent of a pixel) does not necessarily reveal the susceptibility of the iron that might be contained within that voxel: a small amount of high-susceptibility (and presumably high-toxicity) paramagnetic iron might yield the same magnetic moment and overall susceptibility as a large amount of low-susceptibility (and presumably low-toxicity) paramagnetic iron.
Resolving this ambiguity requires knowing not just the magnetic moment produced by the material (which MRI can give us) but also the amount of magnetizable material involved. Brammerloh and colleagues obtained this information by separately determining the amount of iron in each voxel via two other techniques: proton-induced x-ray emission and x-ray fluorescence.
Importantly, the researchers achieved this result with single-cell resolution, which required them to overcome additional challenges since cells are smaller than typical MRI voxel sizes. To do that, the team used an ultrahigh-field MRI scanner to reduce the voxel size, bringing it closer to the size of a single cell. Even so, the magnetic field of the iron in just one cell is so weak that its influence may not extend over more than a voxel or two. This complicates the interpretation of the iron susceptibility measurements because of “partial volume effects” (artifacts due to the signal’s dependence on the precise location of the cell relative to the imaging voxel grid). Fortunately, in the studied samples the iron-containing neurons are well separated from one another. This allowed the researchers to locate the neurons of interest with an uncertainty far smaller than the voxel size by fitting the image data with signals predicted by describing the iron sources as isolated magnetic dipoles—an accurate approximation in the far field (see Fig. 1).
Combining this form of superresolution MRI microscopy with measurements of iron quantity obtained from proton-induced x-ray emission and x-ray fluorescence, the researchers make the impressive claim of being able to measure the susceptibility of iron contained within individual human dopaminergic neurons in postmortem brain tissue samples. Interestingly, whereas most iron in cells is thought to be stored in ferritin, for the dopaminergic neurons examined, the team instead found iron primarily bound to low-affinity sites. This observation suggests a higher iron toxicity in dopaminergic neurons than previously presumed.
More work needs to be done to validate these results, as the current investigation was performed on only two test samples. But if the findings hold, the new method may help advance MRI exploration of iron toxicity and contribute to the development of possible new MRI-readable biomarkers for earlier detection of various neurodegenerative diseases.
References
- C. C. Winterbourn, “Toxicity of iron and hydrogen peroxide: The Fenton reaction,” Toxicol. Lett. 82-83, 969 (1995).
- M. Brammerloh et al., “In situ magnetometry of iron in human dopaminergic neurons using superresolution MRI and ion-beam microscopy,” Phys. Rev. X 14, 021041 (2024).
- B. Drayer et al., “Magnetic resonance imaging of brain iron,” Am. J. Neuroradiol. 7, 373 (1986), https://www.ajnr.org/content/7/3/373.
- E. M. Haacke et al., “Imaging iron stores in the brain using magnetic resonance imaging,” Magn. Reson. Imag. 23, 1 (2005).
- J. Acosta-Cabronero et al., “In vivo MRI mapping of brain iron deposition across the adult lifespan,” J. Neurosci. 36, 364 (2016).
- K. Shmueli et al., “Magnetic susceptibility mapping of brain tissue in vivo using MRI phase data,” Magn. Reson. Med. 62, 1510 (2009).
- Y. Wang and T. Liu, “Quantitative susceptibility mapping (QSM): Decoding MRI data for a tissue magnetic biomarker,” Magn. Reson. Med. 73, 82 (2014).